MEDICAL DIRECTIVE
COMFORT CARE / DO NOT RESUSCITATE (“DNR”) ORDER
Commonwealth of Massachusetts
[// GUIDANCE: This template is drafted to meet the Massachusetts Department of Public Health (“DPH”) requirements for a Comfort Care/Do Not Resuscitate Order that is honored by Emergency Medical Services (EMS) and health-care providers statewide. It also embeds best-practice advance-directive language so the document may serve as a standalone DNR directive for facilities that have not yet adopted the standard DPH form. Attorneys should (i) verify that the final execution is on a DPH-approved CC/DNR or MOLST form, or (ii) attach this directive as Schedule A to that form. The statutory citations below are foundational and stable.]
TABLE OF CONTENTS
- Document Header
- Definitions
- Operative Provisions
- Representations & Warranties
- Covenants & Restrictions
- Default, Revocation & Remedies
- Risk Allocation
- Dispute Resolution & Governing Law
- General Provisions
- Execution Block
1. DOCUMENT HEADER
1.1 Title and Parties
This Comfort Care / Do Not Resuscitate Directive (this “Directive”) is made by [PATIENT NAME] (“Patient”), date of birth [DOB], residing at [ADDRESS], in consultation with [AUTHORIZED CLINICIAN NAME & CREDENTIALS] (“Authorized Clinician”) pursuant to 105 MASS. CODE REGS. 170.000 (2024) and Mass. Gen. Laws ch. 201D, § 14 (2024).
1.2 Recitals
A. Patient is of sound mind, has been informed of the nature and consequences of a Do Not Resuscitate order, and voluntarily desires to forego cardiopulmonary resuscitation (“CPR”) in the event of cardiac or respiratory arrest.
B. Authorized Clinician, having evaluated Patient, concurs that a DNR order is medically appropriate.
C. The parties execute this Directive to provide clear, legally enforceable instructions to all health-care providers and EMS personnel.
1.3 Effective Date & Jurisdiction
This Directive becomes effective on [EFFECTIVE DATE] and is governed exclusively by the laws of the Commonwealth of Massachusetts.
2. DEFINITIONS
“Authorized Clinician” means a physician, nurse practitioner, or physician assistant licensed in Massachusetts who signs this Directive.
“Comfort Care” means medical interventions intended to alleviate pain or discomfort without attempting resuscitation.
“CPR” means cardiopulmonary resuscitation, advanced cardiac life support, defibrillation, or other life-sustaining interventions intended to restart or support cardiac or pulmonary function.
“EMS Personnel” means emergency medical technicians and paramedics certified under 105 MASS. CODE REGS. 170.000.
“Good-Faith Standard” means actions taken honestly, without negligence or willful misconduct, consistent with Mass. Gen. Laws ch. 201D, § 14.
“Health-Care Proxy” means any individual appointed under a valid Health Care Proxy instrument to make health-care decisions on Patient’s behalf.
3. OPERATIVE PROVISIONS
3.1 Do Not Resuscitate Order
a. Patient expressly directs that no CPR be attempted if Patient experiences cardiac or respiratory arrest.
b. All other appropriate Comfort Care measures shall be provided.
3.2 Scope of Treatment
This Directive applies in all settings (hospital, skilled nursing facility, home, ambulance, or other) and to all providers, including EMS Personnel.
3.3 Documentation Requirements
a. A copy of this Directive, or the original, shall be kept prominently in Patient’s medical record.
b. Patient [check one] ☐ will ☐ will not obtain and wear a DPH-approved DNR bracelet or necklace.
c. A photocopy or electronic facsimile of a properly executed Directive carries the same legal effect as the original.
3.4 Consideration
The mutual promises herein constitute adequate consideration.
4. REPRESENTATIONS & WARRANTIES
4.1 Patient Representations
a. Capacity: Patient affirms capacity to execute this Directive.
b. Voluntariness: Execution is voluntary and not the result of duress or undue influence.
4.2 Authorized Clinician Representations
a. Licensure: Authorized Clinician is duly licensed and in good standing in the Commonwealth of Massachusetts.
b. Medical Judgment: The DNR order is consistent with prevailing medical standards and Patient’s condition.
c. Compliance: Authorized Clinician will file or transmit this Directive in accordance with facility policy and DPH regulations.
4.3 Survival
The representations and warranties herein survive execution and remain in force until revocation per Section 6.
5. COVENANTS & RESTRICTIONS
5.1 Patient Covenants
a. Notification: Patient will provide copies of this Directive to all current and future health-care providers.
b. Update Obligation: Patient will advise providers promptly if this Directive is revoked.
5.2 Provider Covenant
Authorized Clinician shall review the Directive with Patient at significant changes in medical status.
6. DEFAULT, REVOCATION & REMEDIES
6.1 Revocation by Patient
Patient may revoke this Directive at any time by:
i. Writing “VOID” across this document or the DPH CC/DNR form;
ii. Verbally expressing the intent to revoke in the presence of a health-care provider; or
iii. Executing a superseding DNR directive or order.
6.2 Effect of Unauthorized Resuscitation
Resuscitative measures provided contrary to this Directive do not constitute revocation. Patient retains all other rights under law, including the right to withdraw or withhold other treatments.
6.3 Remedies
The parties acknowledge that (i) specific performance and injunctive relief are the primary and adequate remedies for breach, and (ii) monetary damages would be inadequate.
7. RISK ALLOCATION
7.1 Indemnification of Providers
Patient (and, if applicable, Patient’s estate) releases and agrees to indemnify and hold harmless all health-care providers and EMS Personnel who, in good-faith reliance on this Directive, withhold CPR in accordance with its terms, to the fullest extent permitted by Mass. Gen. Laws ch. 201D, § 14.
7.2 Limitation of Liability
No health-care provider or EMS Personnel acting under this Directive in good faith shall incur civil or criminal liability.
7.3 Insurance
[// GUIDANCE: Insert any facility-required professional-liability language here.]
8. DISPUTE RESOLUTION & GOVERNING LAW
8.1 Governing Law
This Directive is governed by and construed in accordance with the laws of the Commonwealth of Massachusetts, without regard to conflict-of-law principles.
8.2 Forum Selection
Because this is a health-care directive rather than a commercial contract, forum selection and arbitration are inapplicable. Any judicial proceeding shall be brought in a court of competent jurisdiction in Massachusetts.
8.3 Injunctive Relief
Nothing herein limits Patient’s or a provider’s right to seek emergency injunctive relief to enforce or challenge the Directive.
9. GENERAL PROVISIONS
9.1 Amendment
Amendments must be in writing, signed by Patient and Authorized Clinician, and compliant with 105 MASS. CODE REGS. 170.000.
9.2 Assignment
This Directive is personal to Patient and is not assignable.
9.3 Severability
If any provision is held invalid, the remaining provisions shall remain in full force to the maximum extent permissible.
9.4 Integration
This Directive constitutes the complete agreement regarding CPR and supersedes all prior inconsistent statements or documents, except a duly executed DPH CC/DNR or MOLST form, which shall control if attached.
9.5 Counterparts & Electronic Signatures
This Directive may be executed in counterparts and delivered by electronic signature, each deemed an original.
10. EXECUTION BLOCK
[// GUIDANCE: Massachusetts does NOT require notarization for a DNR order. Two adult witnesses are recommended (and required for a Health Care Proxy) but not strictly mandated for a CC/DNR. Include them for belt-and-suspenders protection, especially in institutional settings.]
10.1 Patient
_______________________________________
[PATIENT NAME]
Date: _________________________________
10.2 Authorized Clinician
_______________________________________
[AUTHORIZED CLINICIAN NAME & CREDENTIALS]
License No.: ___________________________
Facility/Practice: ______________________
Date: __________________________________
10.3 Optional Witnesses
Witness 1:
_______________________________________
Name: ________________________________
Date: ________________________________
Witness 2:
_______________________________________
Name: ________________________________
Date: ________________________________
ATTACHMENTS
• Schedule A – Copy of Massachusetts DPH Comfort Care / DNR Verification Form (if executed separately)
• Schedule B – Copy of any valid Health Care Proxy
[// GUIDANCE: Final Checklist for Counsel
1. Print on brightly-colored paper (e.g., pink) if required by facility policy for EMS visibility.
2. Confirm that Schedule A is the latest DPH CC/DNR or MOLST form (current version available on the DPH website).
3. Upload a copy into the patient’s electronic medical record and provide copies to the health-care proxy, primary care physician, and local EMS provider.
4. Advise Patient to carry a reduced-size copy in wallet/purse and consider a bracelet/necklace.
5. Re-evaluate the Directive whenever the patient’s condition or goals of care change.]
© [YEAR] [LAW FIRM/ATTORNEY NAME]. All rights reserved.
Do more with Ezel
This free template is just the beginning. See how Ezel helps legal teams draft, research, and collaborate faster.
AI that drafts while you watch
Tell the AI what you need and watch your document transform in real-time. No more copy-pasting between tools or manually formatting changes.
- Natural language commands: "Add a force majeure clause"
- Context-aware suggestions based on document type
- Real-time streaming shows edits as they happen
- Milestone tracking and version comparison
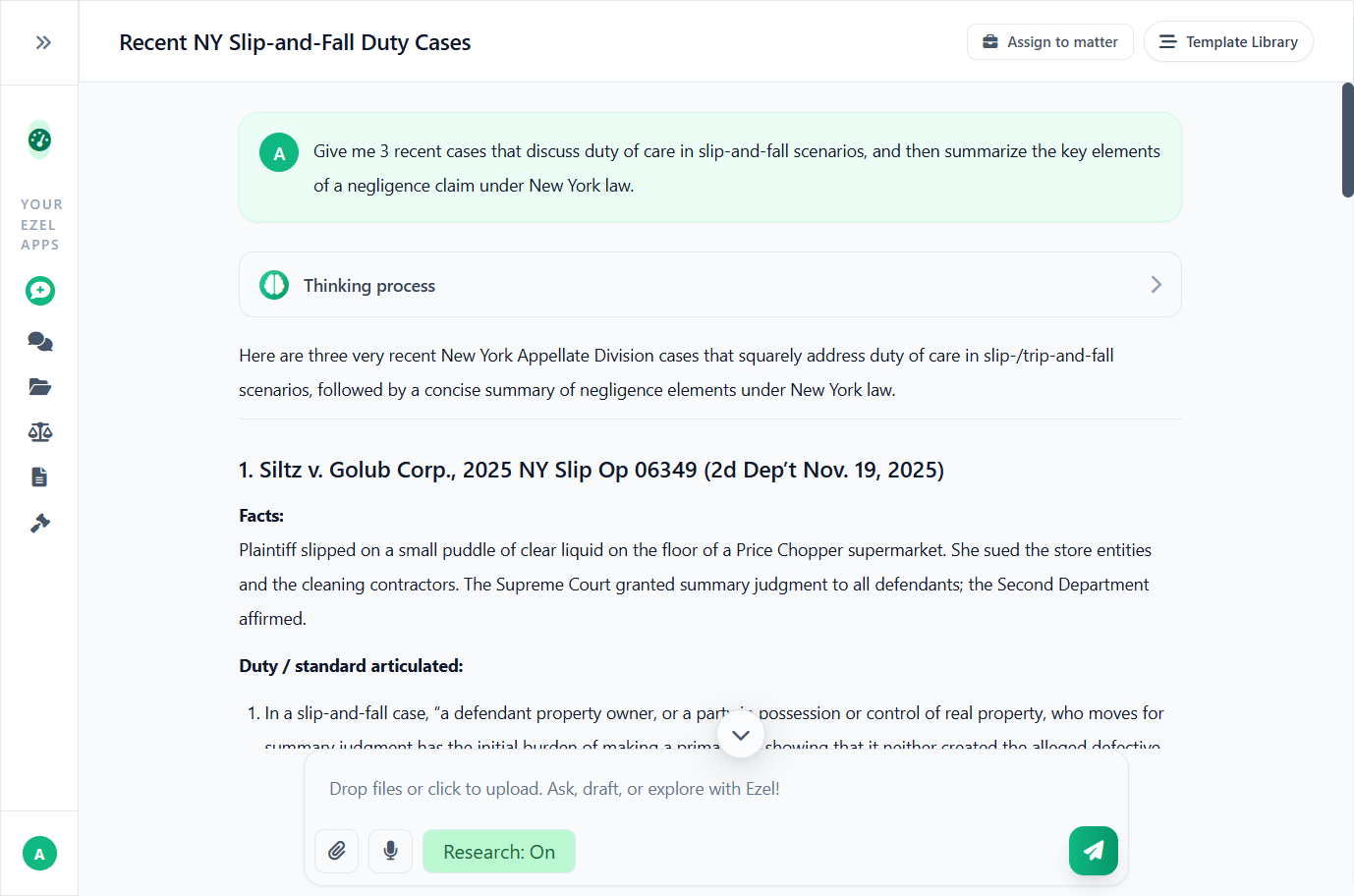
Research and draft in one conversation
Ask questions, attach documents, and get answers grounded in case law. Link chats to matters so the AI remembers your context.
- Pull statutes, case law, and secondary sources
- Attach and analyze contracts mid-conversation
- Link chats to matters for automatic context
- Your data never trains AI models
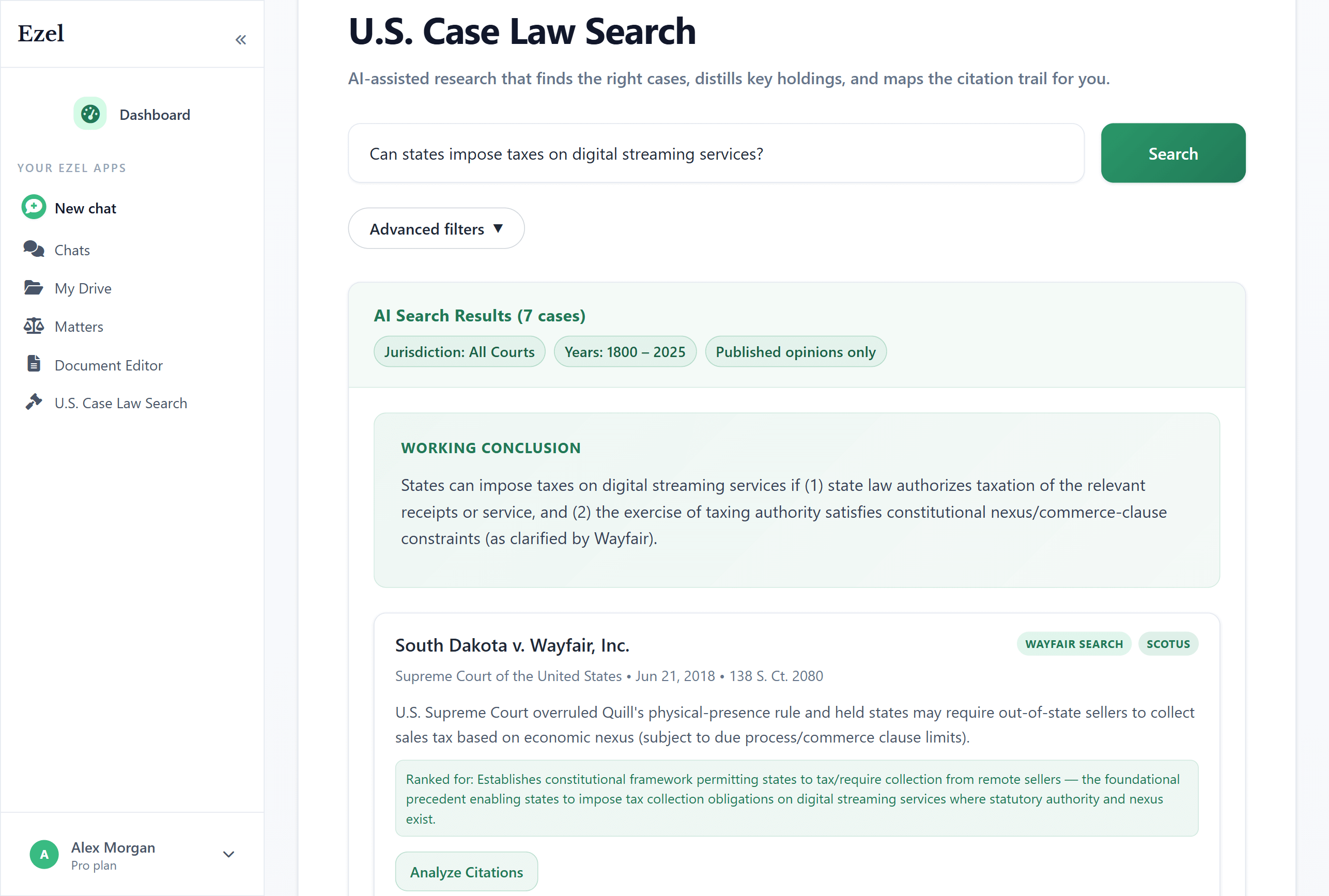
Search like you think
Describe your legal question in plain English. Filter by jurisdiction, date, and court level. Read full opinions without leaving Ezel.
- All 50 states plus federal courts
- Natural language queries - no boolean syntax
- Citation analysis and network exploration
- Copy quotes with automatic citation generation
Ready to transform your legal workflow?
Join legal teams using Ezel to draft documents, research case law, and organize matters — all in one workspace.