OKLAHOMA OUT-OF-HOSPITAL
DO-NOT-RESUSCITATE (DNR) ORDER & ADVANCE MEDICAL DIRECTIVE
(Okla. Stat. tit. 63, § 3131 et seq.)
[// GUIDANCE: This template is designed to comply with the Oklahoma Do-Not-Resuscitate Act and related health-care decision statutes. Bracketed items must be customized. Omit brackets in final execution copy. Text appearing in ALL-CAPS is statutorily prescribed language and should not be altered absent compelling clinical reasons.]
TABLE OF CONTENTS
- Document Header ……………………………………………………………….. 2
- Definitions ……………………………………………………………………………… 3
- Operative Provisions ………………………………………………………………. 4
- Representations & Warranties ………………………………………………… 6
- Covenants & Restrictions ………………………………………………………… 6
- Revocation, Default & Remedies ……………………………………………… 7
- Risk Allocation ……………………………………………………………………… 8
- Miscellaneous / General Provisions ………………………………………… 9
- Execution Block & Required Witness / Notary Statements …………… 10
- EMS Recognition Acknowledgment ……………………………………… 12
1. DOCUMENT HEADER
1.1 Title
THIS OUT-OF-HOSPITAL DO-NOT-RESUSCITATE ORDER & ADVANCE MEDICAL DIRECTIVE (this “Directive”) is executed pursuant to the Oklahoma Do-Not-Resuscitate Act, codified at Okla. Stat. tit. 63, § 3131 et seq. (the “Act”).
1.2 Parties
(a) “Patient”: [PATIENT FULL LEGAL NAME], an individual born [DOB], presently residing at [ADDRESS].
(b) “Attending Physician”: [PHYSICIAN NAME, M.D./D.O., LICENSE NO.], whose principal practice address is [ADDRESS] (the “Physician”).
(c) “Health-Care Providers & EMS Personnel”: Any person or entity providing medical care or emergency services to the Patient.
1.3 Effective Date
This Directive becomes effective on the later of (i) the date all signatures required in Section 9 are affixed, or (ii) [EFFECTIVE DATE] (the “Effective Date”).
1.4 Governing Law
All matters arising under or relating to this Directive shall be governed by, and construed in accordance with, the health-care laws of the State of Oklahoma, without regard to conflict-of-laws principles.
2. DEFINITIONS
For purposes of this Directive, the following capitalized terms shall have the meanings set forth below; all references to statutory terms incorporate the definitions provided in the Act unless otherwise indicated.
“Act” – The Oklahoma Do-Not-Resuscitate Act, Okla. Stat. tit. 63, § 3131 et seq.
“Advanced Cardiac Life Support” or “ACLS” – External chest compressions, endotracheal intubation, defibrillation, administration of cardiac drugs, or any other medical interventions intended to restart or sustain cardiac or respiratory function.
“Comfort Care” – Medical or nursing interventions designed to alleviate pain or provide comfort, including but not limited to oxygen, analgesics, suctioning, or positioning, expressly excluding ACLS.
“Good Faith” – Honesty in fact and the reasonable belief that the action is warranted by the Directive and applicable law.
“Patient Representative” – A health-care proxy, legal guardian, attorney-in-fact under a durable power of attorney for health care, or other surrogate decision-maker authorized under Oklahoma law.
“Resuscitative Measures” – Collectively, ACLS and any other clinical interventions intended primarily to revive or sustain cardiac or respiratory function.
“Revocation” – Any act described in Section 6.1 effectuating a withdrawal of the Directive’s authority.
[// GUIDANCE: Add additional defined terms as necessary for institutional policies.]
3. OPERATIVE PROVISIONS
3.1 Directive Not to Resuscitate
SUBJECT TO COMFORT CARE, THE PATIENT HEREBY DIRECTS THAT IN THE EVENT THE PATIENT SUFFERS A CARDIAC OR RESPIRATORY ARREST, NO RESUSCITATIVE MEASURES SHALL BE INITIATED.
3.2 Scope of Non-Resuscitation Order
(a) Resuscitative Measures Prohibited. Health-Care Providers and EMS Personnel shall withhold or withdraw all Resuscitative Measures, including but not limited to:
i. External chest compressions;
ii. Endotracheal intubation or advanced airway management;
iii. Defibrillation or cardioversion;
iv. Intravenous cardiac medications intended to restart or sustain cardiac function.
(b) Measures Permitted. The following shall remain available unless separately refused by the Patient:
i. Comfort Care;
ii. Hemostatic or palliative interventions necessary to alleviate pain;
iii. Nutrition and hydration (unless refused in writing elsewhere).
[// GUIDANCE: If the Patient wishes to refuse additional treatments—e.g., artificial nutrition—attach a supplemental schedule.]
3.3 Conditions Precedent
This Directive applies only when the Patient is (i) outside an acute-care hospital setting OR in a hospital but elects to use this statutory DNR order; and (ii) experiences cardiac or respiratory arrest.
3.4 Obligations of Health-Care Providers
(a) Verification. Providers must confirm the presence of an original or unrevoked copy of this Directive or an approved DNR bracelet/necklace before withholding Resuscitative Measures.
(b) Documentation. Providers shall document reliance on this Directive in the Patient’s medical record and indicate date, time, and method of verification.
(c) Transfer Protocols. Receiving facilities must be furnished a copy of this Directive upon transfer.
3.5 Consideration
The mutual promises herein and the statutory immunities afforded under the Act constitute adequate consideration.
4. REPRESENTATIONS & WARRANTIES
4.1 Patient
(a) Capacity. The Patient represents that he/she has decision-making capacity OR that the undersigned Patient Representative has lawful authority to act.
(b) Voluntariness. Execution of this Directive is voluntary and not the product of duress or undue influence.
4.2 Physician
The Physician warrants that:
(a) He/She has explained the medical consequences of executing this Directive;
(b) The Patient (or Patient Representative) appeared to understand the information provided;
(c) The Physician has no reason to believe the Directive conflicts with any known expressed wishes of the Patient.
4.3 Survival
All representations and warranties survive execution and remain effective until Revocation or expiration per Section 6.2.
5. COVENANTS & RESTRICTIONS
5.1 Affirmative Covenants
(a) Patient Covenant. The Patient agrees to carry or wear evidence of this Directive (original form, medic-alert bracelet, or necklace).
(b) Physician Covenant. The Physician shall, upon request, provide additional signed copies for inclusion in the medical chart and for EMS use.
5.2 Negative Covenants
No Health-Care Provider or EMS Personnel shall initiate Resuscitative Measures contrary to the express terms of this Directive, except as allowed under Section 6 (Revocation) or as otherwise required by law.
5.3 Notice Obligations
The Patient or Patient Representative shall promptly notify the Physician and primary caregivers of any Revocation.
6. REVOCATION, DEFAULT & REMEDIES
6.1 Revocation Methods
This Directive may be revoked at any time by:
(a) A written, dated, and signed revocation delivered to the Physician or any Health-Care Provider;
(b) An oral statement expressing the intent to revoke, made by the Patient or authorized Patient Representative, in the presence of a witness age 18 or older;
(c) The physical destruction of the Directive and all duplicates by the Patient or Patient Representative; or
(d) Execution of a subsequent, conflicting DNR or advance directive.
6.2 Automatic Termination
This Directive automatically terminates upon the earlier of:
(a) Written notice of termination by the Physician;
(b) Discovery that the Patient is pregnant, unless the Patient specifically elects otherwise under Oklahoma law; or
(c) Expiration of [EXPIRATION DATE OR “NONE”] if an expiration is elected.
6.3 Remedies & Enforcement
(a) Injunctive Relief. The Patient (or estate) reserves the right to seek injunctive relief to prevent or correct any actual or threatened violation.
(b) Attorney Fees. A prevailing party in any action to enforce this Directive shall be entitled to reasonable attorney fees and costs.
6.4 Good-Faith Defense
Health-Care Providers or EMS Personnel acting in Good Faith reliance on a facially valid Directive shall be immune from civil or criminal liability to the fullest extent permitted under the Act.
7. RISK ALLOCATION
7.1 Indemnification – Provider Protection
The Patient (and the Patient’s successors, heirs, and assigns) agrees to indemnify, defend, and hold harmless Health-Care Providers and EMS Personnel from any claims, damages, or liabilities arising out of their Good-Faith compliance with, or reliance upon, this Directive.
7.2 Limitation of Liability – Good-Faith Standard
No Health-Care Provider or EMS Personnel shall be liable for any act or omission made in Good Faith pursuant to this Directive, except for gross negligence or willful misconduct.
7.3 Insurance
Nothing herein shall be construed to require any Health-Care Provider to maintain insurance beyond professional liability coverage required by applicable law.
7.4 Force Majeure
Compliance is excused where performance is impossible due to circumstances beyond a provider’s reasonable control (e.g., mass-casualty event, equipment failure), provided the provider exercises reasonable efforts to honor the Directive when feasible.
8. MISCELLANEOUS / GENERAL PROVISIONS
8.1 Entire Agreement
This Directive constitutes the entire agreement respecting the subject matter and supersedes all prior DNR orders unless expressly incorporated herein.
8.2 Amendments & Waivers
Any amendment must be in writing, signed by the Patient (or Patient Representative) and Physician, and witnessed/notarized in accordance with Section 9. No waiver shall be effective unless in writing and signed by the waiving party.
8.3 Assignment
The rights and duties under this Directive are personal and may not be assigned, delegated, or transferred except as provided by law.
8.4 Severability
If any provision is held invalid or unenforceable, the remaining provisions shall remain in full force to the maximum extent permitted.
8.5 Counterparts & Electronic Signatures
This Directive may be executed in counterparts, each of which shall be deemed an original. Photocopies, facsimiles, and electronically signed copies shall be treated as originals.
9. EXECUTION BLOCK & REQUIRED WITNESS / NOTARY STATEMENTS
[// GUIDANCE: Oklahoma law requires EITHER (i) two qualified adult witnesses OR (ii) acknowledgment before a notary public. The witness qualifications below track statutory requirements.]
9.1 Patient or Patient Representative
Signature: _______________________________ Date: _______________
Printed Name: [PATIENT OR REPRESENTATIVE NAME]
Relationship to Patient (if Representative): [RELATIONSHIP]
Capacity Declaration (if Representative):
☐ Health-Care Proxy ☐ Durable POA for Health Care ☐ Legal Guardian ☐ Other: ___________
9.2 Attending Physician
Signature: _______________________________ Date: _______________
Printed Name: [PHYSICIAN NAME], M.D./D.O.
Oklahoma Medical License No.: [LICENSE NO.]
Telephone: [PHONE]
9.3 Qualified Witnesses (Use only if not using a Notary)
Witness #1
I am at least 18 years of age, not related to the Patient by blood or marriage, not entitled to any portion of the Patient’s estate, and not directly involved in the Patient’s health-care provision.
Signature: _______________________________ Date: _______________
Printed Name: ____________________________
Witness #2
[I make the same declaration as Witness #1.]
Signature: _______________________________ Date: _______________
Printed Name: ____________________________
9.4 Notary Acknowledgment (Use in lieu of Witnesses)
State of Oklahoma County of ________________
On this _____ day of ______________, 20____, before me, the undersigned Notary Public, personally appeared [NAME OF SIGNATORY], known to me (or satisfactorily proven) to be the person whose name is subscribed above, and acknowledged that he/she executed the same for the purposes therein contained.
Notary Public Signature: __________________________
Printed Name: ___________________________________
My Commission Expires: ___________________________
(Seal)
[// GUIDANCE: The Patient may elect either witness or notary execution, but NOT both. Strike out unused subsection.]
10. EMS RECOGNITION ACKNOWLEDGMENT
THE PATIENT AND PHYSICIAN ACKNOWLEDGE THAT EMS PERSONNEL IN OKLAHOMA ARE AUTHORIZED TO RELY UPON:
(a) THE ORIGINAL OF THIS DIRECTIVE OR A CLEAR PHOTOCOPY;
(b) A STATE-APPROVED DNR BRACELET OR NECKLACE ISSUED PURSUANT TO THE ACT; OR
(c) AN ELECTRONIC IMAGE TRANSMITTED BY A HEALTH-CARE FACILITY’S STANDARD PROCEDURES,
PROVIDED SUCH DOCUMENT OR DEVICE IS READILY AVAILABLE AT THE SCENE.
[// GUIDANCE (FINAL CHECKLIST):
• Print the executed Directive on brightly colored paper (commonly orange) for rapid EMS identification.
• Provide copies to the Patient’s primary care physician, preferred hospital(s), and each home-health or hospice agency involved.
• Encourage the Patient to carry a wallet-sized card referencing this Directive.
• Recommend periodic review, especially upon changes in health status, residence, or treatment preferences.]
END OF DOCUMENT
Do more with Ezel
This free template is just the beginning. See how Ezel helps legal teams draft, research, and collaborate faster.
AI that drafts while you watch
Tell the AI what you need and watch your document transform in real-time. No more copy-pasting between tools or manually formatting changes.
- Natural language commands: "Add a force majeure clause"
- Context-aware suggestions based on document type
- Real-time streaming shows edits as they happen
- Milestone tracking and version comparison
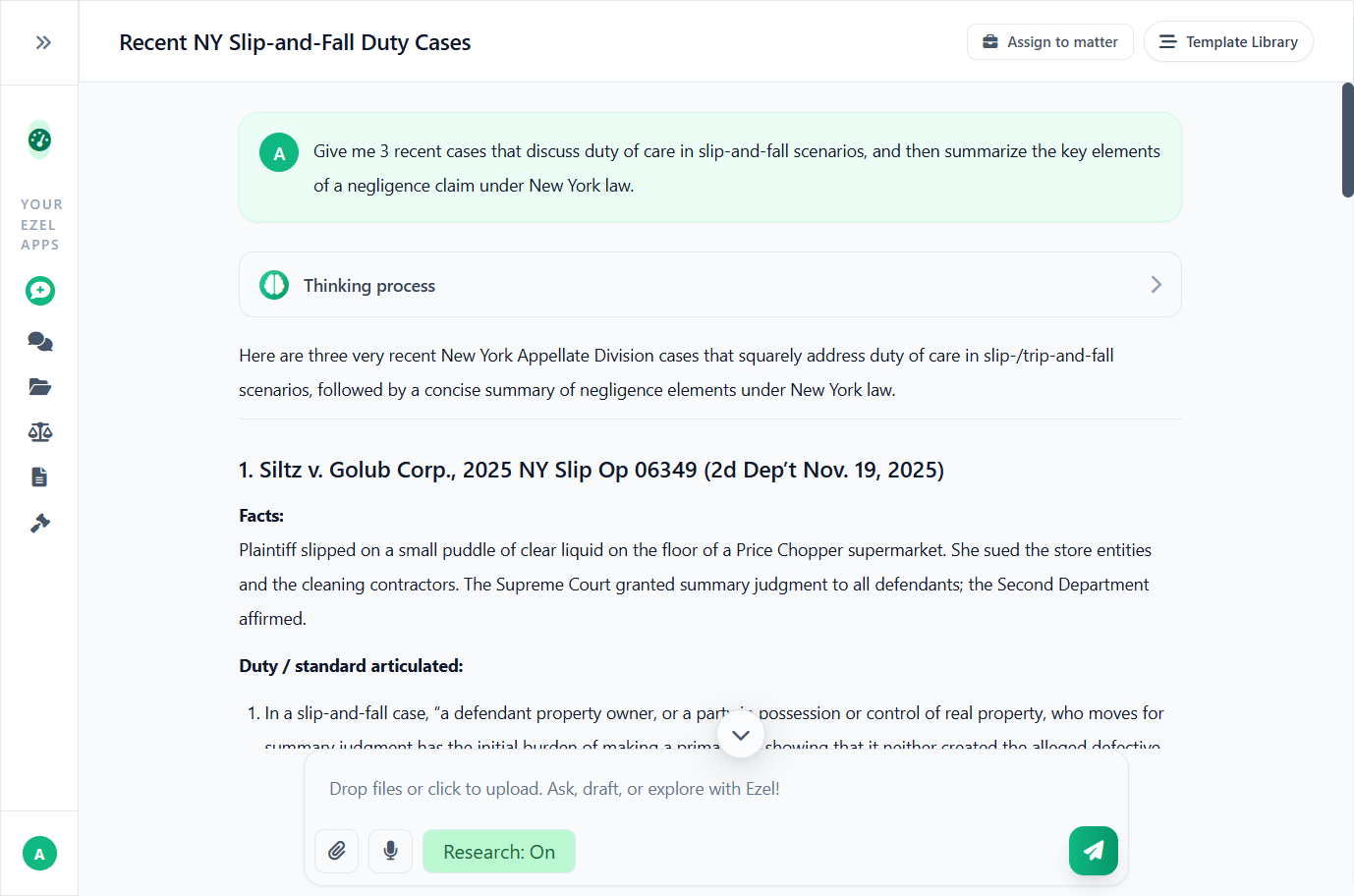
Research and draft in one conversation
Ask questions, attach documents, and get answers grounded in case law. Link chats to matters so the AI remembers your context.
- Pull statutes, case law, and secondary sources
- Attach and analyze contracts mid-conversation
- Link chats to matters for automatic context
- Your data never trains AI models
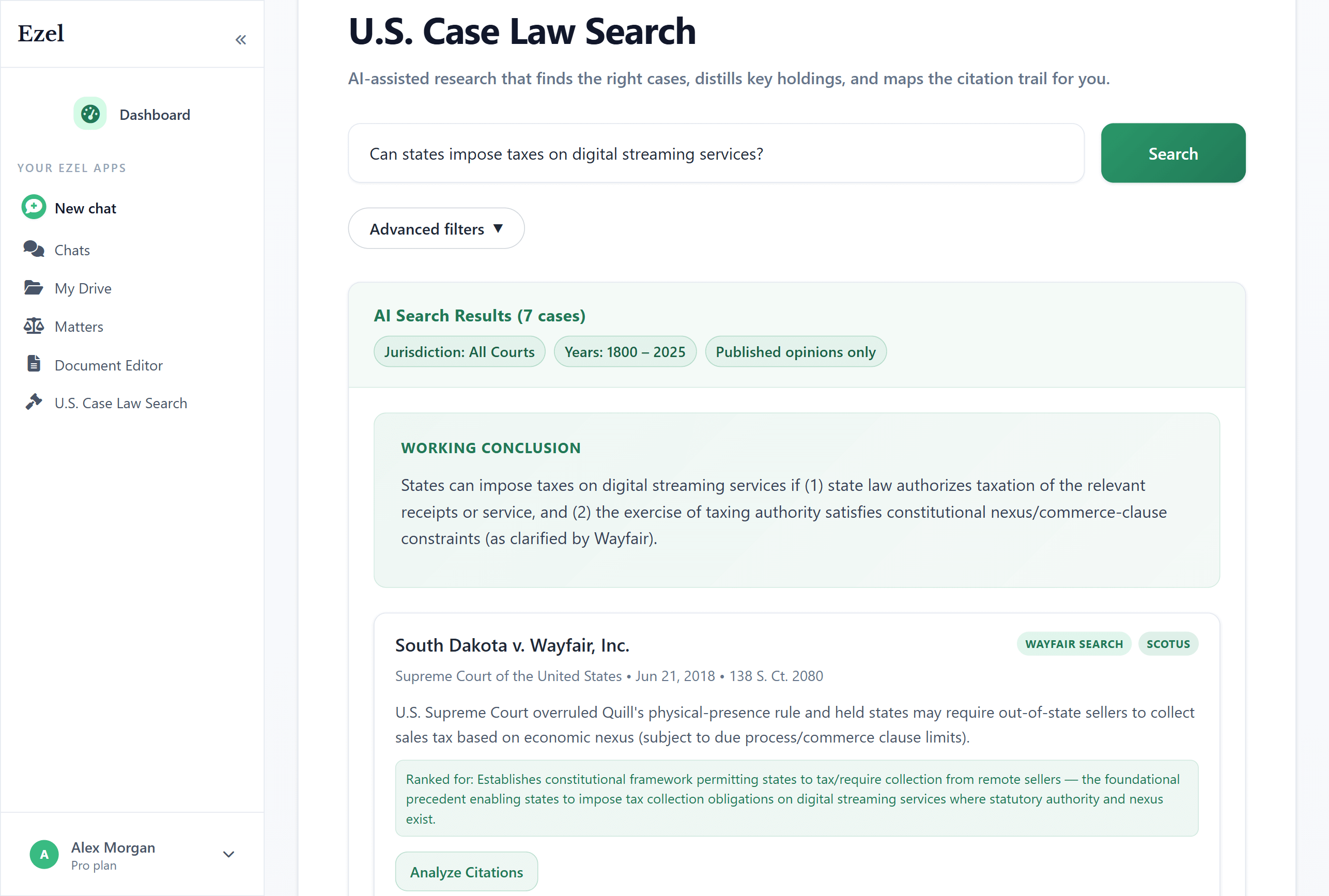
Search like you think
Describe your legal question in plain English. Filter by jurisdiction, date, and court level. Read full opinions without leaving Ezel.
- All 50 states plus federal courts
- Natural language queries - no boolean syntax
- Citation analysis and network exploration
- Copy quotes with automatic citation generation
Ready to transform your legal workflow?
Join legal teams using Ezel to draft documents, research case law, and organize matters — all in one workspace.